Heartburn after a meal? A sour taste creeping up your throat at night? You’re not alone. Around 20% of Singapore’s population experiences gastroesophageal reflux disease (GERD), a chronic condition that can cause heartburn, regurgitation and discomfort.
For many, lifestyle changes and medication can help. But when symptoms persist or complications are suspected, your doctor may recommend an endoscopy to get a clearer look at what’s going on inside. This guide explains when an endoscopy may be recommended, what the procedure involves, and how it can help in diagnosing and managing GERD.
Role of Endoscopy in Diagnosing GERD
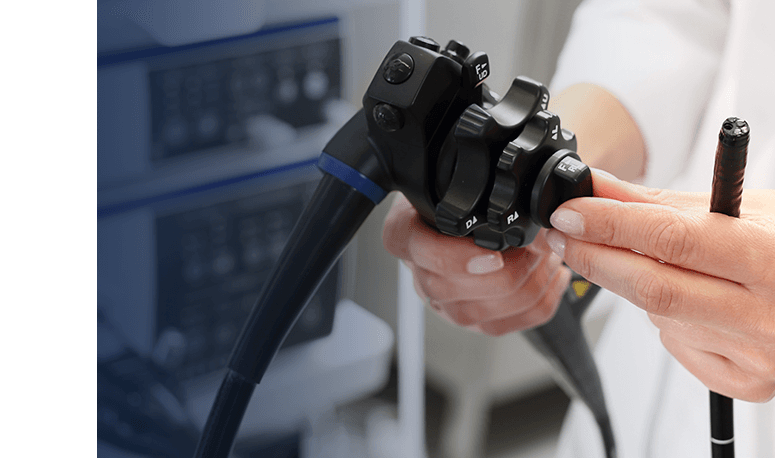
An upper endoscopy, also known as oesophagogastroduodenoscopy (OGD), is a procedure that uses a thin, flexible tube with a camera (endoscope) to visualise the upper digestive tract. This helps doctors to directly inspect the lining of these organs for signs of GERD, such as inflammation (oesophagitis), erosions, ulcers or Barrett’s oesophagus.
Beyond visual assessment, endoscopy allows for tissue sampling through biopsy when necessary. These samples can be analysed microscopically to confirm diagnoses, rule out other conditions and monitor for precancerous changes. The procedure also enables therapeutic interventions, such as dilation of strictures or treatment of bleeding lesions.
When Is Endoscopy Recommended for GERD?
Not everyone with GERD needs an endoscopy. If your symptoms are mild and respond well to medication, your doctor may not recommend it right away. However, if your symptoms are persistent, unusual, or accompanied by warning signs, an endoscopy can help identify complications or other causes.
You may be advised to undergo endoscopy if you experience:
- Difficulty swallowing (dysphagia) or painful swallowing (odynophagia) – This helps identify strictures, inflammation, or other structural changes in the oesophagus.
- Unintentional weight loss – To rule out more serious conditions, such as cancer.
- Signs of anaemia (e.g., fatigue, dizziness, shortness of breath) – An endoscopy can reveal potential bleeding in the gastrointestinal tract.
- Hoarseness or chronic cough – Examination can determine whether acid reflux is irritating or damaging the throat or vocal cords.
- Throat discomfort or chest pain – Helps detect inflammation or structural issues in the oesophagus.
- Palpable abdominal mass – Identify abnormal growths or tumours in the upper digestive tract.
- Vomiting blood or blood in stool – Used to locate the source of gastrointestinal bleeding.
If you have Barrett’s oesophagus or another GERD-related complication, your doctor may recommend periodic endoscopy to monitor for changes over time.
Preparing for an Upper Endoscopy
Preparing for an endoscopy involves several steps to ensure safety and effectiveness. Before the procedure, your doctor will review your medical history, current medications, and any existing health conditions. Be sure to mention anything important, such as bleeding disorders, allergies, or medications you take regularly, so your care team can plan safely.
You’ll also receive a few important instructions to follow before your appointment:
Medication Adjustments
Certain medications, such as blood thinners or nonsteroidal anti-inflammatory drugs (NSAIDs), may need to be stopped or adjusted days before the procedure to reduce bleeding risks. Always follow your doctor’s advice and do not stop medications without guidance.
Fasting
You will usually be asked to avoid food and drinks for several hours before your procedure. Having an empty stomach supports optimal visualisation and reduces the risk of complications.
Transportation Arrangements
Since sedation is usually given, you will not be able to drive home afterward. Arrange for someone to accompany you or help with transport after your appointment.
How Does an Endoscopy Work?
An upper endoscopy usually takes about 15 to 30 minutes and is done in a day procedure setting. You will be asked to lie on your side, and sedation or a local anaesthetic will be given to keep you comfortable.
The doctor then gently guides the endoscope through your mouth and down into the oesophagus, stomach, and duodenum. The camera sends live images to a screen, allowing a clear view of the digestive lining. Sometimes, air is introduced to expand the area slightly for better visibility.
If any unusual areas are found, your doctor may take small tissue samples for testing. This process is painless and helps ensure an accurate diagnosis. After that, you’ll be taken to a recovery area to rest briefly while the sedation effect subsides.
What to Expect After Endoscopy
After the procedure, patients are monitored for 30–60 minutes until the sedation wears off. Mild throat discomfort, bloating, or gas may occur for a few hours but usually resolve quickly.
Before you leave, your doctor will share the initial findings and explain what was observed during the procedure. If a biopsy was taken, the results will be ready in a few days. Most people can return to normal activities the next day.
While complications are uncommon, do reach out to your doctor right away if you experience chest pain, difficulty breathing, fever, or trouble swallowing after the procedure. These symptoms are rare but should be checked promptly.
Alternative Tests to Endoscopy for GERD Diagnosis
An endoscopy provides valuable information, but it’s not the only way doctors assess GERD. Depending on your symptoms, your doctor may recommend other tests to better understand your condition:
Ambulatory Oesophageal pH Monitoring
This test involves placing a small probe with a pH sensor through the nostril into the oesophageal lining to measure acid exposure over 24 hours. It helps confirm acid reflux in patients with normal endoscopy results or atypical symptoms.
Oesophageal Manometry
This procedure checks how well the muscles in your oesophagus and lower oesophageal sphincter are working. By measuring pressure changes as you swallow, it can reveal whether a motility disorder might be causing or worsening your reflux symptoms.
Barium Swallow
For this X-ray study, you’ll be asked to drink a liquid containing barium. The barium coats your oesophagus, allowing the radiologist to see its shape and movement clearly on imaging. Although it does not show the fine details that an endoscopy does, it can help identify structural issues such as a hiatal hernia or narrowing that may contribute to GERD.
If you have been struggling with frequent heartburn or other discomfort, it’s best to speak with a specialist to find the most suitable treatment plan for your needs.
With over 30 years of experience, our doctors specialise in providing endoscopy services in Singapore with precision and minimal discomfort. They ensure accurate screening results to support the early detection and management of GERD. Book a consultation today to know whether endoscopic evaluation could benefit your specific situation.